SOAP Note AI
Learn to write effective SOAP notes in psychiatry with this comprehensive guide. Enhance patient care and documentation skills.
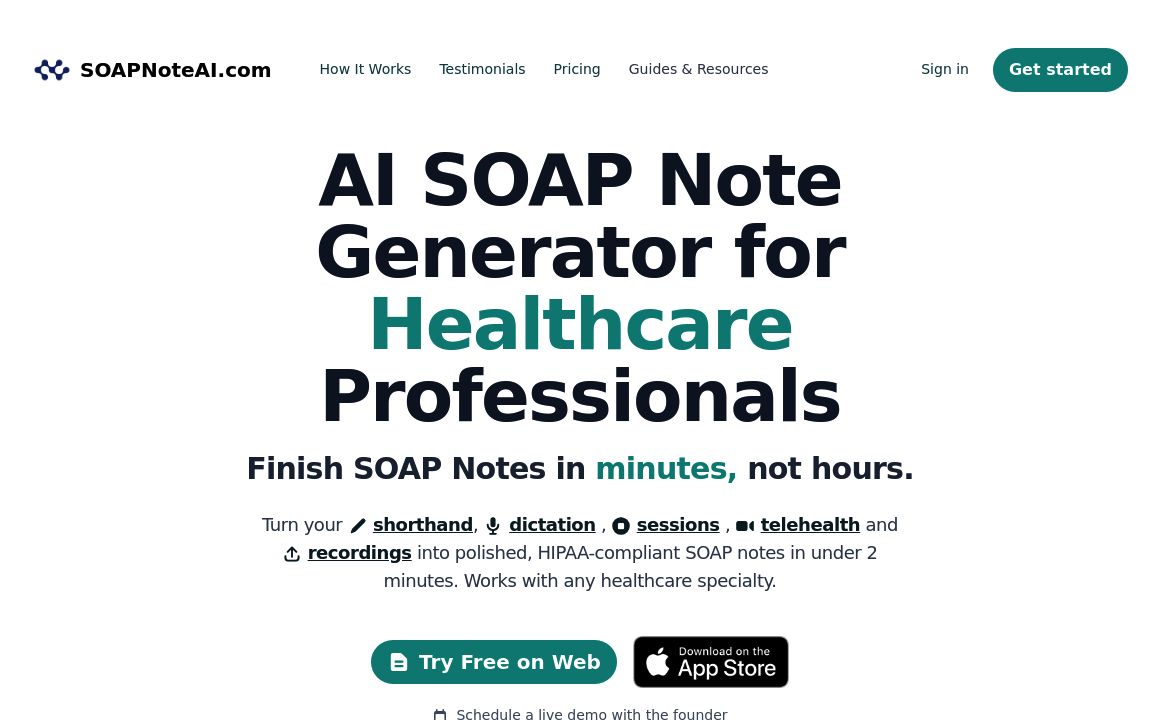
SOAP Note AI's Top Features
Frequently asked questions about SOAP Note AI
Category
HealthcareTop SOAP Note AI Alternatives
Discover Jessica, the AI-powered speech therapist offering 24/7 personalized therapy with advanced s...
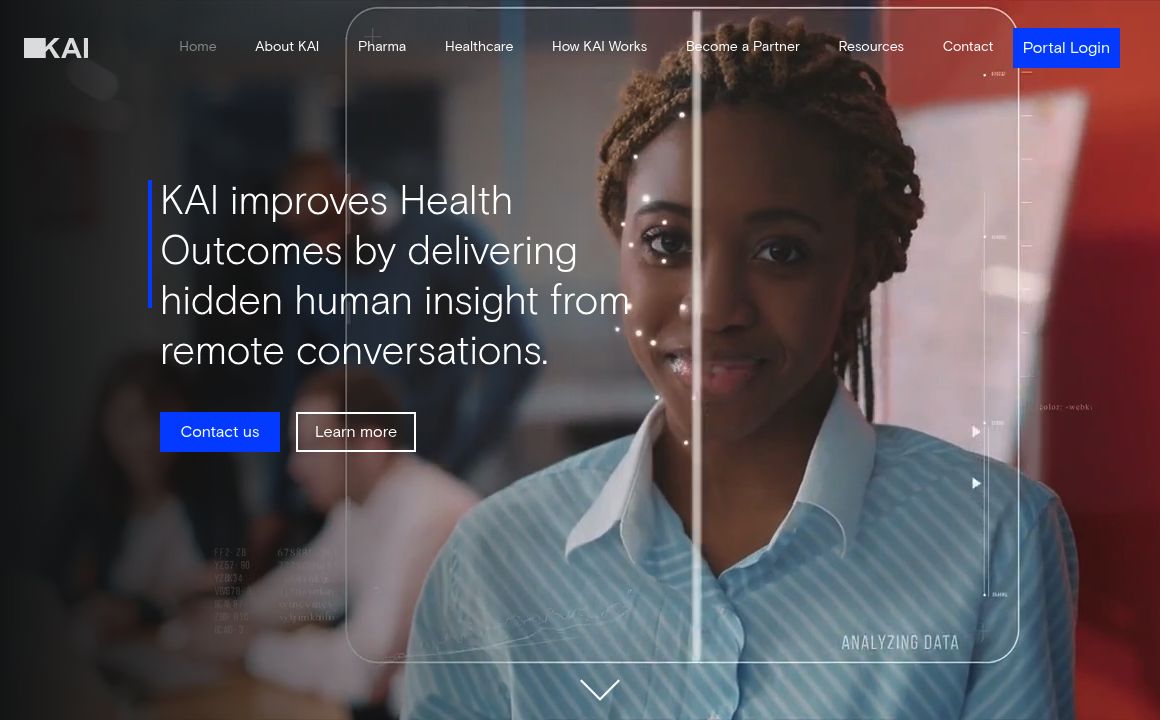
Discover how KAI's Healthcare Services improve remote patient care by providing enhanced insights fo...
proudP
0Explore the proudP App for tailored content for men and doctors, including publications, articles, a...
MediNav
0Discover top doctors and hospitals with ease on MediNav. Your premier source for healthcare navigati...
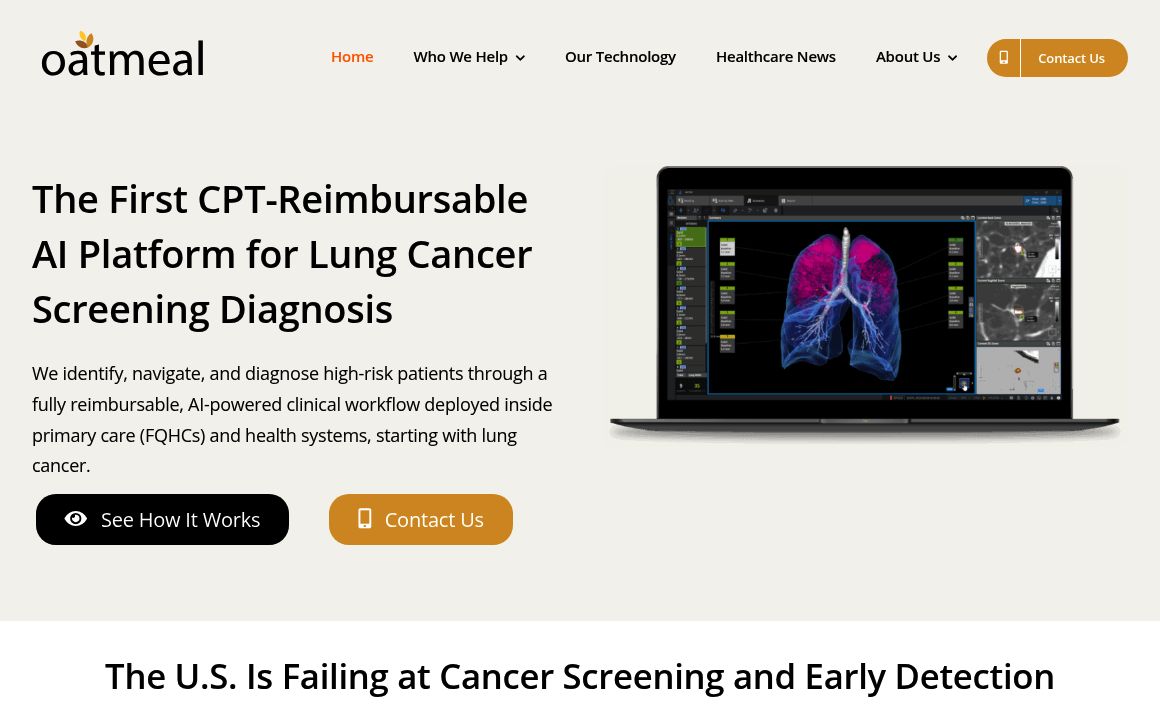
AI-driven cancer screening platform for underserved FQHC patients offering expert primary care, comp...
Ask AI Vet offers speedy, AI-generated answers to veterinarian questions, providing initial advice a...